IMMUNOHAEMATOLOGY - BLOODGROUPSEROLOGY AND COMPATIBILITY
I have already discussed the function of an erythrocyte.
But now I reached the royal discipline of transfusion medicine - Immunohaematology.
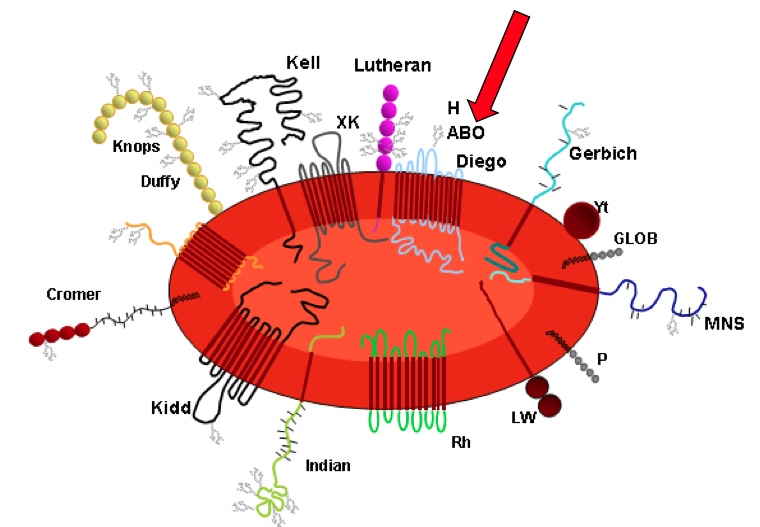
Those completely inconspicuous little discs or unfinished doughnuts swim around, squeeze in everywhere to deliver the oxygen and take the CO2 back with them. They don't even have a cell nucleus. As an "average doctor", I greatly respected what these little miracle buggers do. They squeeze into every capillary, even the smallest, to exchange the gases. But my idea was: cell membrane - somewhat strange shape, but necessary for "squeezing through", a cytoskeleton to keep this peculiar shape and then a lot of haemoglobin... that's it. And even under the microscope, the little buggers don't look very impressive. And I only thought a little about blood groups (what they are or where they are). And I'm pretty sure doctors with little to do with blood (ophthalmologists, sports doctors, general practitioners) have a similar idea of erythrocytes. And here comes the great revelation! There are countless molecules on these little discs. They are enzymes, proteins, carbohydrates, transporters or simple molecules of which we still have no idea what they do "for a living". There are currently 376 of these molecules defined. 343 of them are assigned to 43 blood group systems. For 33, the genetics are not yet known. Seven new blood group systems have been added since 2019 alone. And these substances are all blood groups - not just the A and B, but 376. So for me, it was, to put it mildly, a "bit of a surprise" :-).
Of course, the newly discovered blood group antigens do not play a significant role clinically. They are either antigens that we all possess. With these antigens, the absence is the abnormality. Or they can be antigens that are found by chance in someone. These antigens are rare (very rare) and have no significance for the owner.
From the perspective of a blood transfusion specialist, the first scenario is much more critical. This is because if a patient who lacks a high-frequency antigen develops an antibody to that antigen - following a transfusion, pregnancy, or other natural occurrences - it becomes challenging to supply them with compatible blood. In such cases, the patient's relatives are tested, and ideally, the patient should store their own blood for future use. Unfortunately, this is rarely feasible as only a few blood banks can store autologous blood. In Austria, this service is only available in Vienna.
The picture below shows some of the blood groups schematically, but these are not all.
The most important blood group system is the ABO system. It includes four main blood groups, which are defined by two antigens and two antibodies.
Blood group A is the most common in Europe, with about 43%. The erythrocytes have antigen A on their surface, and the antibodies against blood group B are found in the plasma.
With blood group B, which is one of the rarest with approx. 11%, the B antigen is found on the surface of the erythrocytes, and antibodies against blood group A are in the plasma.
Blood group O is the second most common, with 41%, and the erythrocytes have neither the A nor the B antigen on their surface. In contrast, antibodies against both antigens are found in serum.
Blood group AB is the rarest (5%). The erythrocytes have both antigens; no antibodies are found in the plasma.
Special features:
- Antibodies against the blood group antigens develop during the first 6 months of life. One theory explains the formation of these antibodies by immunisation against intestinal bacteria that have similar structures to the A and B antigens. According to the Landsteiner rule, however, we can only form antibodies against structures we do not have and know, so someone with blood group A does not develop antibodies against bacteria with antigen A-like structures. They only form antibodies against bacteria with antigen B-like structures. With blood group B, it is the other way around.
- Anti-A and anti-B antibodies belong to the natural (regular) antibodies, also called isoagglutinins. They mainly belong to the IgM antibodies and are more effective at RT or lower. Some of the antibodies in blood group O belong to the IgG antibodies. In addition, some of the antibodies have the specificity anti-AB and cannot be separated into A or B.
- According to the current knowledge, antigens A and B are carbohydrates and have no function.
The presence of these natural antibodies was why the ABO system was first to be discovered and why it is the most relevant system for us. The first attempts at blood transfusion usually ended fatally. Most likely, the donor did not have a compatible blood group.
Karl Landsteiner discovered the different properties of serum and red cells, which he described in his paper "Ueber Agglutinationserscheinungen normalen menschlichen Blutes." He determined three blood groups: A, B, and C, which later became BG O. Landsteiner was awarded the Nobel Prize in Medicine in 1930 for his discovery.
Blood can be transfused if it is identical or compatible with the recipient's blood group. It's important to make sure the recipient doesn't have any antibodies against the donor's red blood cells. This is known as major compatibility. Minor compatibility means the donor doesn't have antibodies against the recipient's blood group antigens. With standard blood products, the minor compatibility is no longer significant because only a small amount of the donor's plasma remains in the red cell concentrate. This small amount of antibodies in the donor's blood bag may react with the recipient's red blood cells, but it's at such a low level that it's not measurable and doesn't have any clinical impact.
Whole blood transfusions must match the patient's blood group since plasma makes up a large portion of the transfusion. While whole blood transfusions are now less common, they are still regularly used in research, particularly in war zones, where using whole blood is preferred over giving individual blood components (red blood cells, plasma, and platelets) in massive transfusions.
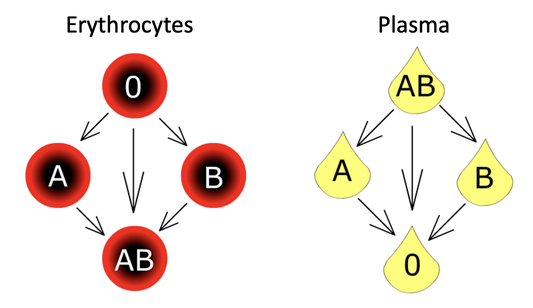
Thus, considering the antigen-antibody combinations listed above, we get the following donor scheme:
An individual with BG O is a universal donor, and an individual with blood group AB is the universal recipient. It is the opposite with plasma - blood group O is the universal recipient, and blood group AB is the universal donor.
This is the donor scheme for erythrocytes and for plasma:
RelevanCE fOr THE CliniCIAN
Prior to the transfusion of a red blood cell concentrate (blood unit), the individual administering the transfusion must conduct a bedside test. Up until August 2016, this responsibility was solely carried out by medical personnel. However, an amendment to the law in August 2016 expanded the authority to administer blood products to senior nursing staff.
Please ensure to conduct the bedside test to double-check the compatibility of the red cell concentrate with the patient. This test specifically covers the ABO system. It is a quick test to determine the blood group of the red cell concentrate and the patient. In order to interpret the test correctly, it's important to understand how it works and which blood group it indicates. Additionally, one must be aware of the compatibility rules. While we always aim to transfuse blood of the same blood group, in cases of irregular antibodies or extensive transfusions, if there is no suitable blood unit available in the patient's blood group, we may need to switch to another compatible blood group. The compatibility rules can be found in the diagrams provided. For erythrocyte concentrates, please refer to the diagram on the left.
BUT THAT'S NOT ALL... 😊
There are 42 other blood group systems - and this number should only be taken with caution - new antigens are found every few months that also acquire the significance of a system.
The ABO system has been and remains the most important for the clinician. But understanding what Rhesus neg or pos means is not a mistake. Especially gynaecologists should know a bit more about it.
The clinician does not need to know all the other blood group systems. But he or she should be aware that there is more, and if there is a patient who is "difficult to transfuse", the clinician can also understand what it means.
Zuletzt bearbeitet am 02.07.2024.
